Systemic lupus erythematosus, commonly known as lupus, is a chronic autoimmune disease that can affect various parts of the body, including the skin, joints, kidneys, heart, lungs, brain, and blood cells and mouth. It primarily affects women, usually developing between the ages of 15 and 44.
Key points about systemic lupus erythematosus include:
• Autoimmune Nature: SLE occurs when the immune system mistakenly attacks healthy tissues, leading to inflammation and damage in multiple organs and systems.
• Symptoms: The symptoms of SLE can vary widely and may include fatigue, joint pain, skin rashes (such as the characteristic butterfly rash on the face), fever, chest pain, shortness of breath, headaches, cognitive difficulties, and sensitivity to sunlight.
Here are some key points regarding SLE and oral health:
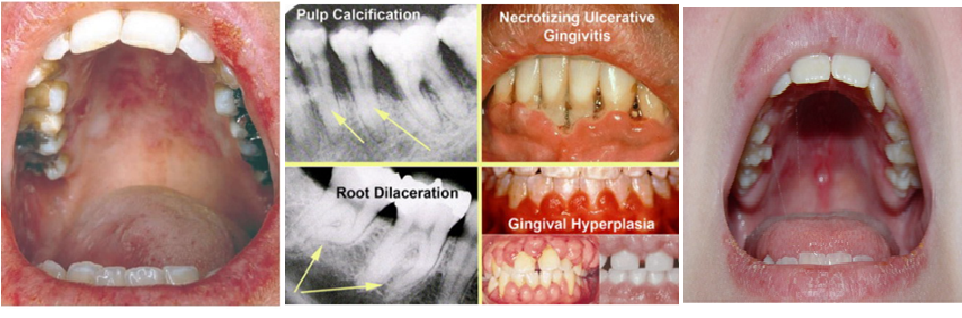
• Oral Ulcers: One of the most common oral manifestations of SLE is the presence of oral ulcers. These ulcers are typically painless and can occur on the lips, buccal mucosa (inner cheeks), palate, or gums. They may appear as white or red patches with a surrounding border.
• Dry Mouth (Xerostomia): SLE can cause a reduction in saliva production, leading to dry mouth. Dry mouth can increase the risk of dental problems such as tooth decay, gum disease, oral infections, and difficulty in speaking and swallowing.
• Gingivitis and Periodontitis: Individuals with SLE may be at an increased risk of developing gingivitis (gum inflammation) and periodontitis (gum disease). Proper oral hygiene, regular dental check-ups, and professional cleanings are essential to prevent and manage these conditions.
• Temporomandibular Joint (TMJ) Disorders: SLE can also affect the temporomandibular joints, which are the joints that connect the jawbone to the skull. TMJ disorders can cause jaw pain, difficulty in opening or closing the mouth, clicking or popping sounds, and problems with biting and chewing.
Diagnosis: Diagnosing SLE can be challenging due to the diversity of symptoms. Medical history, physical examination, blood tests (such as antinuclear antibody test and specific antibody tests), and imaging studies may be used to support the diagnosis
Treatment: The goal of treatment is to control symptoms, prevent flare-ups, and minimize organ damage. It typically involves a combination of medications, including nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, antimalarial drugs, immunosuppressants, and biologic agents. Additionally, lifestyle modifications, such as sun protection and regular exercise, can be beneficial.
Medications and Oral Health: Some medications used to manage SLE, such as corticosteroids and immunosuppressants, can have oral health implications. For example, long-term use of corticosteroids may increase the risk of oral infections and delayed wound healing.
Flare-ups and Remission: SLE is characterized by periods of flare-ups (active disease) followed by periods of remission (low disease activity or absence of symptoms). Managing stress, getting enough rest, and adhering to treatment plans are essential for minimizing flare-ups.
Long-Term Outlook: The prognosis for SLE varies depending on the severity and extent of organ involvement. With appropriate treatment and regular medical care, many individuals with SLE can lead active and productive lives.
Dental Care: It is important for individuals with SLE to maintain good oral hygiene practices, including regular brushing, flossing, and visiting the dentist for routine check-ups. It's also recommended to inform your dentist about your SLE diagnosis and any medications you are taking. In some cases, prophylactic antibiotics may be necessary before dental procedures to prevent infection.
In conclusion, individuals with SLE should be aware of the potential oral health implications of the disease and the medications used to manage it. Regular dental check-ups and good oral hygiene practices are essential for maintaining oral health and preventing complications.
Our Doctors
SMILE IN MINUTES Dental Care Doctors

Dr. Priyanka
Sr. Dental Surgeon

Dr. Mowmita Barik
Dental Surgeon (BDS)

Dr. Sapna
Dental Surgeon (BDS)

Dr. Md. Shoaib
Dental Surgeon (BDS)
Dr. Rubiya
Dental Surgeon (BDS)

Dr. Kuldeep
Dental Surgeon (BDS)

Dr. Ribhu
Dental Surgeon (BDS)

Dr. Sonam Tonger
Dental Surgeon (BDS)

Dr. Chanderalata
Dental Surgeon (BDS)

Dr. Neha
Dental Surgeon (BDS)
Dr. Priyanka Arora Sethi
Dental Surgeon (BDS)